Feline lungworm and heartworm
Lungworm and heartworm are an underestimated but potentially serious threat for many cats, as this article reveals.
Published 13/10/2022
Also available in Français , Deutsch , Italiano , Polski , Română and Español
Hypertrophic cardiomyopathy is prevalent in the pet cat population, but affected animals may not be easy to identify; this paper offers a comprehensive overview of the condition for the first-opinion veterinarian.

Hypertrophic cardiomyopathy (HCM) is the most prevalent cardiomyopathy in cats, characterized by left ventricular hypertrophy and reduced diastolic function.
Detection of a murmur, arrhythmia or gallop sound in an asymptomatic cat always warrants further cardiac investigations.
Echocardiography is the gold standard diagnostic tool, with assessment of left atrial size being an important prognostic indicator.
HCM has a variable progression and often has a long pre-clinical phase; staging offers prognostic information and helps determine the need for treatment or altered management.
Feline hypertrophic cardiomyopathy (HCM) is a primary myocardial disease defined by left ventricular (LV) concentric hypertrophy, i.e., thickening of the LV walls 1. It is a disease of diastolic dysfunction (impaired relaxation), normally with preserved systolic function (contractility). The reduced compliance of the myocardium affects the ability of the heart to relax and fill during diastole, with consequent increased diastolic pressure, resulting in progressive left atrial (LA) dilation 2. HCM is a diagnosis of exclusion, with the need to rule out other possible cardiac or systemic diseases which may be causing or contributing to a HCM phenotype, such as systemic hypertension, hyperthyroidism, acromegaly and aortic stenosis. The disease progression is highly variable, and often has a prolonged asymptomatic, pre-clinical phase which frequently goes undetected. Cats may subsequently present with signs of congestive heart failure (CHF), arterial thromboembolism (TE) or arrhythmias 2,3.
HCM is the most common feline cardiomyopathy, estimated to affect 14.5-34% of the “healthy” cat population 1,4. Domestic short- and longhair cats account for most cases 4, but pedigree breeds with a predilection for HCM include Persians, British Shorthair, Maine Coon, Ragdoll, Sphynx, Himalayan and Bengal. Any age may be affected, but purebred cats in particular may present with severe disease at a young age 4. HCM is over-represented in male cats, accounting for 75% of cases, despite no sex-linked heritable pattern being identified.
Catheryn Partington
Familial HCM in Maine Coon, Ragdoll and Sphynx cats 5,6,7 is a result of mutations in sarcomeric proteins, but in all other cats the cause remains unknown, although it is likely heritable in other purebreds. The sarcomere is the contractile component of cardiomyocytes, with mutations to sarcomeric proteins resulting in altered sarcomere structure and function which ultimately lead to impaired cardiomyocyte performance. The exact process by which sarcomere dysregulation leads to the HCM phenotype is complex and not fully understood. Changes in calcium sensitivity, mechanical function and cell stress culminate in myocyte hypertrophy, collagen synthesis and myocyte disarray – the histopathological hallmarks of feline HCM 4,8.
Two different mutations to the myosin binding protein C in the sarcomere have been identified in Maine Coons and Ragdolls (A31P and R820W respectively) 5,6. Individuals heterozygous for the mutation often have subclinical disease, with changes only at a cellular, not gross, level, but homozygote cats are more severely affected; an incomplete dominance mode of inheritance is suspected. Maine Coons without the mutation can still develop a HCM phenotype, reflecting the likely multifactorial etiology of the condition. More recently a mutation in the ALMS1* gene has been identified as a causative factor for HCM in Sphynx cats 7.
* ALMS1 = Alstrom syndrome 1
As noted above, HCM manifests as LV hypertrophy and diastolic dysfunction, whereby pathological changes reduce the ventricle’s ability to relax and fill during diastole. Furthermore, progressive hypertrophy of the wall reduces blood supply to the cardiomyocytes, which are replaced by fibrous tissue as they die, further reducing myocardial compliance (i.e., increased stiffness). Consequently, the diastolic pressure within the LV for any given volume of blood increases, in turn increasing pressure within the LA, which then enlarges. Elevated LA pressure is transmitted back to the pulmonary veins, and when pulmonary venous pressure exceeds 25 mmHg, pulmonary edema, the characteristic feature of left-sided CHF, ensues 4. In cats the veins draining the lung pleura open into the pulmonary veins, allowing pleural effusion to develop with left-sided CHF (differing to dogs, in which pleural effusion is always a result of right-sided CHF, never left-sided) 4.
Progressive LA enlargement is one of the factors predisposing cats with severe HCM to thromboembolic disease, although this condition is outwith the scope of this article. The marked hypertrophy, reduced oxygen supply and replacement fibrosis within the myocardium act as substrates for the development of arrhythmias.
LV hypertrophy in feline HCM may affect both the interventricular septum and free wall, or the changes can be asymmetric, with only a focal region affected – typically the base of the interventricular septum. Hypertrophy may also affect the right ventricle, but the pattern and distribution can be highly variable between individuals (Figures 1 and 2) 4. There may also be changes to the mitral valve apparatus, including elongation of the anterior mitral valve leaflet and papillary muscle hypertrophy. Systolic anterior motion (SAM) of the mitral valve is a common feature of HCM and may cause significant left ventricular outflow tract obstruction (LVOTO) 9,10.


Figure 1. The pattern of LV hypertrophy in feline hypertrophic cardiomyopathy can be highly variable between individuals, but both these gross pathology specimens show diffuse left ventricular hypertrophy.
Abbreviation: LVFW, left ventricle free wall; IVS, interventricular septum; RV, right ventricle
Courtesy of Emanuele Ricci, University of Liverpool, UK.

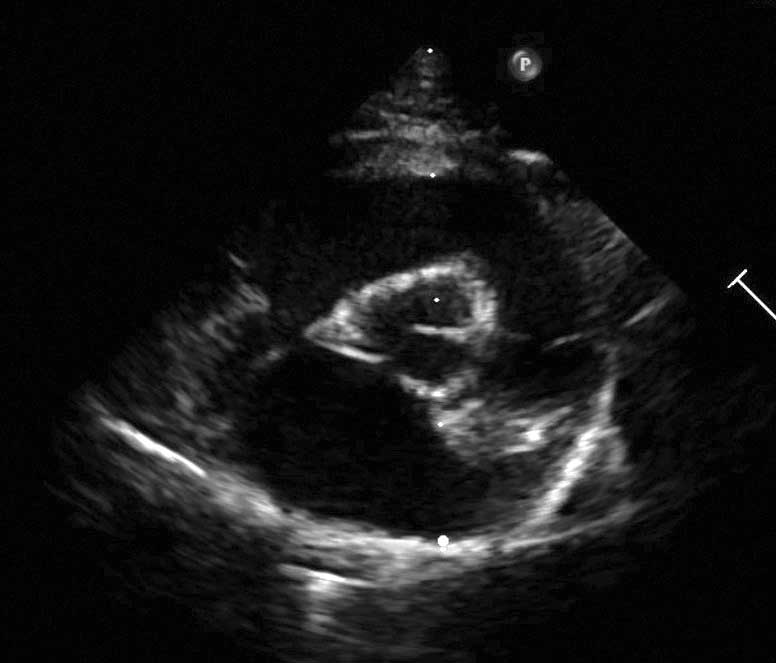
Figure 2a. Echocardiographic views of HCM can show great variability. A right parasternal long axis 5 chamber view showing a focal region of hypertrophy affecting the basal septum (*).
Credit: Catheryn Partington – Joanna Dukes-McEwan

Figure 2b. Echocardiographic views of HCM can show great variability. A right parasternal short axis view at the level of the papillary muscles showing left ventricular and papillary muscle hypertrophy.
Credit: Catheryn Partington – Joanna Dukes-McEwan

Figure 2c. Echocardiographic views of HCM can show great variability. A right parasternal long axis 4 chamber view showing symmetric hypertrophy of the interventricular septum and left ventricular free wall.
Credit: Catheryn Partington – Joanna Dukes-McEwan
Abbreviations: LA, left atrium; LV, left ventricle; Pm, papillary muscle
A subset of cats with HCM may have significant LVOTO (Figure 3). Such cases have classically been termed hypertrophic obstructive cardiomyopathy (HOCM), but human medicine has moved away from this term, as the presence of LVOTO can be intermittent, and as the same is true for cats, the term is likely outdated ,3,9,11. LVOTO may be a result of SAM of the mitral valve, focal hypertrophy of the basal septum, or, less commonly, mid-cavity obstruction due to papillary muscle hypertrophy 4,9,12. This LVOTO causes a murmur due to increased turbulence of blood. With SAM, the obstruction is typically dynamic, worsening with increased cardiac contractility, such as during physical or emotional stress. This is often the reason for variability in the presence or intensity of murmurs in cats with HCM.
SAM of the mitral valve occurs when the septal (anterior) leaflet (often elongated) is pulled towards the outflow tract as a result of hypertrophy and displacement of the papillary muscle, which cause slack chordae tendineae 10. As the outflow tract becomes narrowed by this abnormal movement of the leaflet (or by basal septal hypertrophy), the blood velocity increases and the pressure decreases, dragging the tip of the leaflet further into the outflow tract and worsening the obstruction (the Venturi effect) 4,9. SAM is thought to increase myocardial oxygen demand and reduce coronary perfusion, increasing the risk of myocardial ischemia; it is likely associated with progressive hypertrophy and microvascular dysfunction. It is thought that some cats with severe LVOTO show signs of reduced exercise capacity and angina-type pain, as described in people.

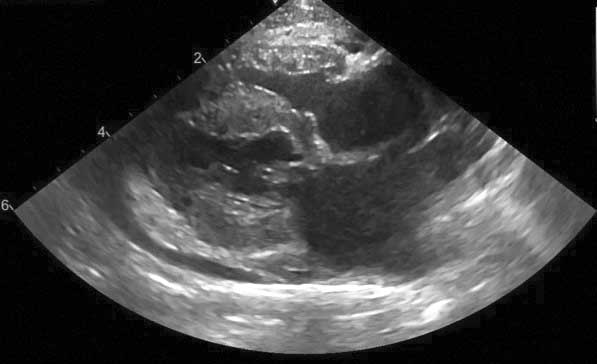
Figure 3a. Murmurs in cats with HCM most often result from left ventricular outflow tract obstruction (LVOTO). A right parasternal long axis 5 chamber view with color flow Doppler showing a turbulent jet of blood flow in the left ventricular outflow tract (open arrow) caused by systolic anterior motion of the mitral valve and a small eccentric jet of mitral regurgitation (small arrow).
Credit: Catheryn Partington – Joanna Dukes-McEwan

Figure 3b. Murmurs in cats with HCM most often result from left ventricular outflow tract obstruction (LVOTO). A right parasternal long axis 5 chamber view showing focal basal septal hypertrophy (*) as a cause of LVOTO.
Credit: Catheryn Partington – Joanna Dukes-McEwan

Figure 3c. Murmurs in cats with HCM most often result from left ventricular outflow tract obstruction (LVOTO). Spectral Doppler of the LVOT showing increased velocities (*) and biphasic acceleration (classic “scimitar” shape), indicative of LVOTO.
Courtesy of J. Novo Matos, University of Cambridge, UK.
Abbreviations: Ao, aorta, LA, left atrium, LV, left ventricle.
Transient myocardial thickening (TMT) is an important differential diagnosis for a HCM phenotype. It is uncommon and poorly understood, but is characterized by increases in LV wall thickness and LA dilation which are less marked than that seen in primary HCM, and there is full resolution of clinical signs and echocardiographic changes over a period of some months. TMT is thus associated with an excellent prognosis. Cats presenting with CHF secondary to TMT tend to be younger than those with primary HCM, and an antecedent event (such as general anesthesia) is often reported. It has been postulated that increased wall thickness is due to myocardial edema, with similarities to both acute myocarditis and stress-induced cardiomyopathy in humans 13.
The recent ACVIM guidelines on the diagnosis and treatment of HCM 14 outline a staging system, similar to that used for myxomatous mitral valve disease in dogs (Box 1). This system can help determine whether treatment is indicated, as well as provide owners with some expectation of what lies ahead – as the progression of HCM, and thus prognosis, is highly variable. In some cats the disease is progressive, leading to CHF, TE and cardiac death, while others may remain pre-clinical and eventually die from non-cardiac causes 14,15. The reason for such heterogenicity remains unclear, and it is difficult to predict which cats may succumb to their disease, although several retrospective studies have identified a number of prognostic factors. Cats diagnosed at a younger age tend to have longer survivals 2. Cats which develop CHF secondary to factors such as stress or intravenous fluid therapy (IVFT) typically have longer survival than other stage C HCM cats. The presence of gallop sounds, arrhythmias, severe LA dilation, reduced LA systolic function, spontaneous echo contrast, severe wall hypertrophy (> 9 mm), LV systolic dysfunction and focal wall thinning are associated with an increased risk of CHF and/or TE 2,15.
Box 1. ACVIM staging of feline HCM.
 |
Stage A |
Stage A: cats predisposed to, but with no current evidence of, HCM; e.g., a Maine Coon with the A31P gene mutation, or a cat with a close relative diagnosed with HCM. The heart will be structurally normal on ultrasound scan. |
 |
Stage B1 |
Stage B: cats with preclinical HCM (i.e., no clinical signs but echocardiographic evidence of HCM). This is further subdivided based on disease severity and risk of CHF and TE.
• Stage B1: low risk of developing CHF or TE, with a normal or mildly dilated LA.
• Stage B2: higher risk of imminent CHF or TE, with moderate to severe dilation of the LA.
|
 |
Stage B2 | |
 |
Stage C | Stage C: cats with clinical signs of HCM and CHF or TE. |
 |
Stage D |
Stage D: HCM cats with CHF refractory to treatment.
|
Credit: Catheryn Partington
Due to the reduced diastolic function and subsequent increase in pressures for any given volume of blood within the LV, cats with HCM are more sensitive to increases in circulating volume (i.e., increased preload). Certain treatments, such as prolonged corticosteroid use and IVFT, could therefore push a cat with advanced HCM into left-sided CHF. This highlights the importance of identifying cats with pre-clinical disease, so that such treatments can be modified and closely monitored (e.g., lower IVFT rates, closer monitoring of respiratory rates, and sequential imaging to assess left atrial size) to reduce risk of decompensation. Furthermore, cats with advanced HCM are at risk of thromboembolism, and identifying these individuals allows initiation of preventative antiplatelet therapy.
Identification of stage B cats may facilitate detection of subtle signs of early progression to stage C, as owners may be better educated and more vigilant regarding the signs of CHF, thus allowing initiation of treatment before there is fulminant pulmonary edema and severe respiratory compromise.
The challenge with HCM is the variable length of the pre-clinical phase, and the frequent lack of any clinical signs or alterations on physical examination. Changes on clinical exam which would raise suspicion of stage B HCM include the presence of a murmur (Box 2), gallop sounds (Box 3) or arrhythmia 4. While many asymptomatic cats with HCM will present with a murmur, upwards of 31-62% will not have a murmur; furthermore, 25-33% of cats with left parasternal systolic murmurs (typically soft, low-grade) have no echocardiographic evidence of a cardiomyopathy 1,4. Louder murmurs (> grade 3/6) are more likely to be associated with significant cardiac disease 4, but any murmur warrants further investigation.
Box 2. Causes of murmurs in pre-clinical HCM.
|
Murmurs are heard when blood flow becomes turbulent; this can be due to high velocity blood flow, large diameter vessels, high fluid density or low viscosity. In HCM murmurs are most often a result of left ventricular outflow tract (LVOT) obstruction due to systolic anterior motion of the mitral valve and/or focal basal septal hypertrophy.
Murmurs in cats with HCM are often dynamic, meaning they may change in intensity, and may even at times be absent. The degree of obstruction is likely worse when the heart contracts with more force (i.e., with increased catecholamines from stress), creating a louder murmur.
|
Box 3. What are gallop sounds?
|
In most healthy cats and dogs only the first (S1) and second (S2) heart sounds are detected on auscultation. A gallop sound is an audible additional heart sound, creating a three-beat cadence, similar to the footfalls of a galloping horse.
This may be due to either an audible third (S3) or fourth (S4) heart sound, although it is often difficult to differentiate between these on auscultation. S3 is a result of rapid ventricular filling in early diastole, whilst S4 is a result of active ventricular filling via atrial contraction in late diastole.
Auscultation of gallop sounds is generally indicative of the presence of diastolic dysfunction, with 2.6-19% of cats with subclinical HCM having a gallop sound 19. They are rarely auscultated in healthy cats, so detection should always prompt further cardiac investigations.
|
Credit: Catheryn Partington – Joanna Dukes-McEwan
Echocardiography is the gold standard for diagnosis of HCM 14, and if hypertrophy is identified, causes of secondary hypertrophy should be investigated. Echocardiography should be advised for any cat with clinical signs possibly attributable to a cardiomyopathy (syncope, exercise intolerance, intolerance to IVFT), those with a familial history of HCM (or sudden death), pedigree cats intended for breeding, and cats where physical exam findings are suggestive of a cardiomyopathy (gallop sounds, arrhythmias, murmur, tachypnea, dyspnea, reduced lung sounds). The ACVIM consensus also advises that cats over 9 years of age undergoing interventions that may precipitate CHF (e.g., general anesthesia, IVFT and prolonged corticosteroid therapy) should also undergo echocardiographic assessment 14.
For the asymptomatic cat, there are four major criteria assessed on echocardiography: LV wall thickness, LA size, presence of LVOTO, and diastolic function. The first two are relatively easily assessed by a general practitioner with basic echo competency in cases with moderate to severe disease.
1. Left ventricular wall thickness
Both the interventricular septum and LV free wall should be assessed, with measurements made on 2-dimensional echocardiography, on right parasternal views at end-diastole (the frame prior to closure of the mitral valve leaflets) (Figure 4a). As hypertrophy can be focal, measurements should be taken over at least three cardiac cycles and ideally from multiple locations. Care should be taken not to include papillary muscles or regions of marked endocardial thickening in wall measurements. An end-diastolic LV wall thickness less than 5 mm is normal, while ≥ 6 mm is consistent with hypertrophy 14. Values of 5-6 mm remain a gray area and should be considered with respect to body size, breed and other echocardiographic variables 16.

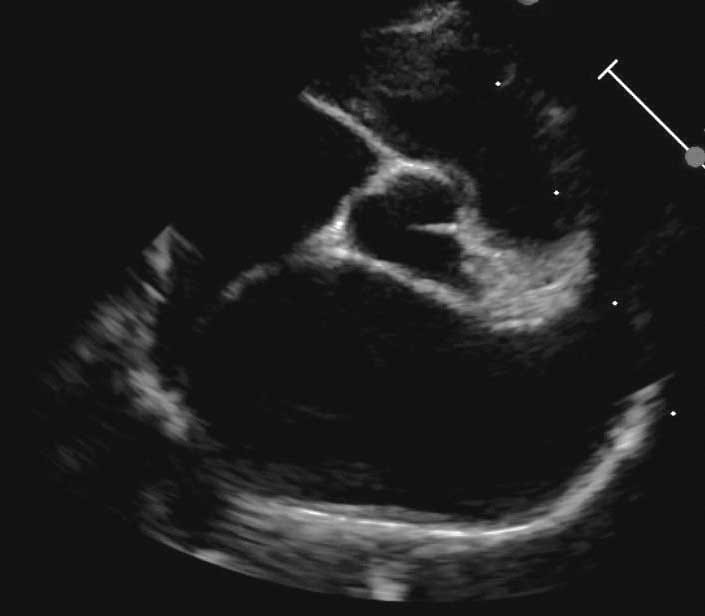
Figure 4a. Echocardiographic assessment of hypertrophic cardiomyopathy (HCM). (a) A right parasternal long axis 5 chamber view. The left ventricular free wall and interventricular septal thickness should be measured on 2 dimensional images in diastole; values ≥ 6 mm are consistent with hypertrophy.
Credit: Catheryn Partington – Joanna Dukes-McEwan
2. Left atrial size
LA size is an independent risk factor for CHF, TE and cardiac death, and can be assessed on both right parasternal long and short axis views. On short axis views at the level of the heart base, measurements are made at early diastole (the frame after closure of the aortic valve cusps), with the atrial diameter being indexed to the aorta (LA/Ao; Figure 4b). The aorta is measured from the midpoint of the convex curvature of the wall of the right aortic sinus to the point where the aortic wall, non-coronary and left coronary aortic cusps merge. The LA is measured from this latter point to the LA free wall, avoiding entering the pulmonary vein 17.

Figure 4b. Echocardiographic assessment of hypertrophic cardiomyopathy (HCM). A right parasternal short axis view at the level of the heart base. The left atrial size is indexed to the aortic root (LA/Ao), measured in early diastole; values > 1.6 are consistent with left atrial dilation.
Credit: Catheryn Partington – Joanna Dukes-McEwan
On the right parasternal long axis four chamber view the LA should be optimized and the left atrial diameter (LAD) measured at end systole (the frame prior to mitral valve leaflet opening), drawing a line parallel to the mitral annulus from the interatrial septum to the LA free wall (Figure 4c) 18. An LA/Ao > 1.6 and LAD > 16.0 mm is consistent with LA enlargement; an LA/Ao > 1.8-2.0 or LAD > 18-19 mm is considered moderate to severe LA enlargement. LA fractional shortening can also be evaluated to assess systolic function. Subjective assessment of the left auricular appendage size, presence of spontaneous echo-contrast or a thrombus, and assessment of left auricular appendage velocities are also important in assessing CHF and TE risk.

Figure 4c. Echocardiographic assessment of hypertrophic cardiomyopathy (HCM). A right parasternal long axis 4 chamber view. The left atrium diameter is measured parallel to the mitral annulus at end systole; values > 16.0 mm are consistent with left atrial dilation.
Credit: Catheryn Partington – Joanna Dukes-McEwan
Abbreviations: Ao, aorta; IVS, Interventricular septum; LA, left atrium; LV, left ventricle; LVFW, left ventricular free wall; MV, mitral valve.
3. Presence of LVOT obstruction
This can be assessed on 2-dimensional, M-mode, color flow and spectral Doppler (Figure 3c). SAM can be visualized on both 2-dimensional and M-mode. Color flow Doppler will highlight turbulence in the LVOT and possibly mitral regurgitation. Spectral Doppler to assess LVOT velocities requires good alignment to flow; with dynamic obstruction the Doppler profile will often show biphasic acceleration (a classic scimitar shape).
4. Diastolic function
Diastolic function can be assessed by both spectral Doppler and Tissue Doppler imaging, but further discussion is beyond the scope of this article. Cats with advanced HCM may also have impaired systolic function.
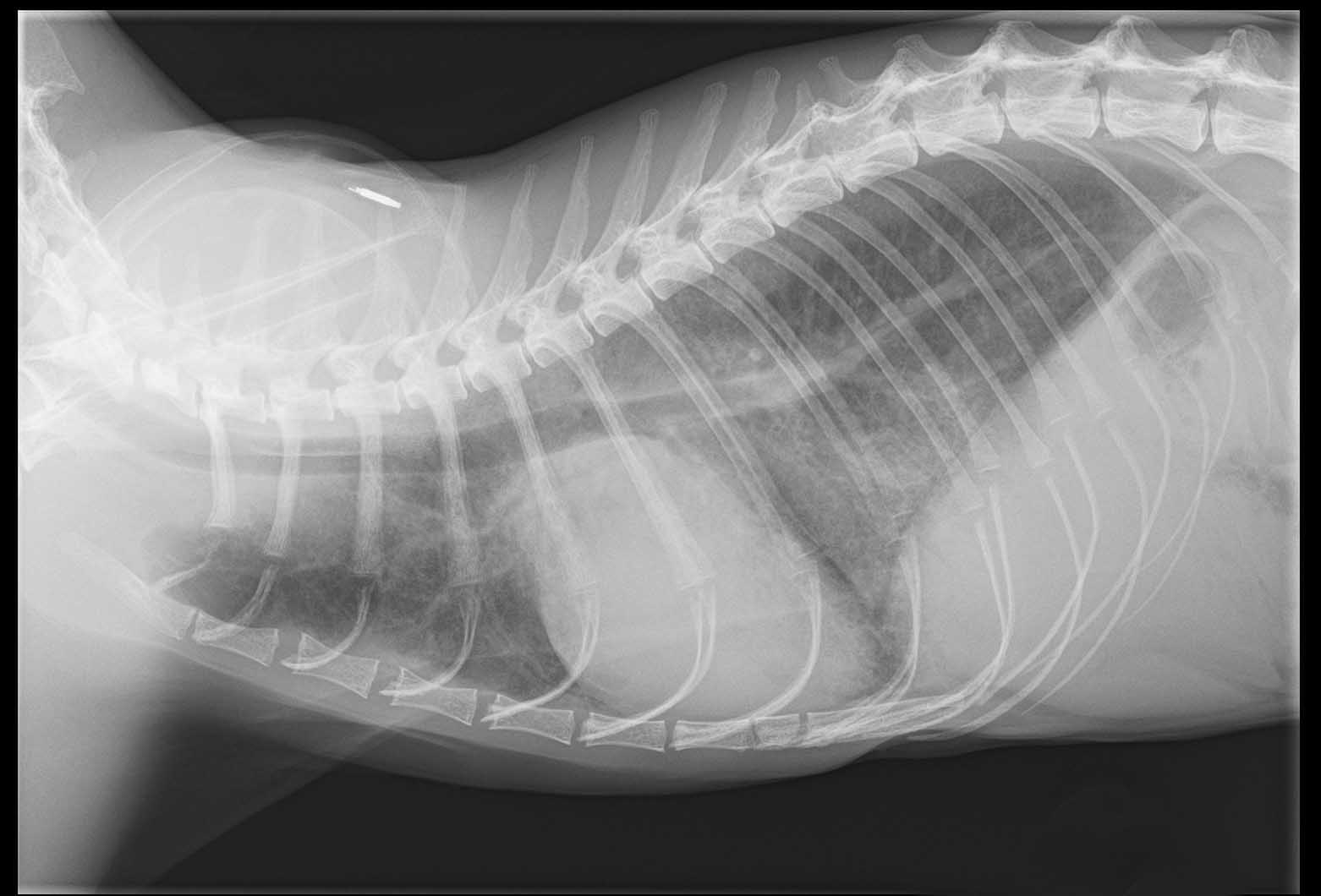
Thoracic radiography is the gold standard for diagnosis of pulmonary edema, but is less useful in asymptomatic cats 14. Severe cardiomegaly with LA bulging may be seen, however radiographs have a lower sensitivity for detection of mild to moderate remodeling in HCM patients, many of which may have a normal cardiac silhouette.
Biomarkers will be discussed in greater detail elsewhere, but in brief these can be a useful tool when used in adjunct to other diagnostics and for monitoring of disease progression, although they should be used with caution as a screening tool. For the asymptomatic cat, quantitative NT-proBNP (a marker of myocardial stress and stretch) has limited use as a screening tool in the general population, as although it has high specificity, the sensitivity is low, meaning a high risk of false negative results. The test is likely better when used selectively in cases of suspected cardiomyopathy (i.e., where a murmur is detected) 19 and along with echocardiography to gain a better understanding of the cardiomyopathy severity. The point-of-care (benchtop) NT-proBNP test is of more use in the symptomatic cat to discriminate between cardiac and non-cardiac causes of dyspnea 20.
Cardiac troponin I (Tn I), a marker of cardiomyocyte injury, is again useful alongside echocardiography, and has been shown to have prognostic significance, with increased values associated with poorer outcomes 21. Myocardial ischemia may result in high levels, which is reported in advanced feline HCM. Severe elevations may raise suspicion of myocarditis causing a secondary HCM phenotype, warranting further investigations.
Both biomarkers have been shown to be higher in cats with HCM and SAM, than in HCM cases without SAM, even in cats with normal/equivocal LA size 22.
Genetic testing is available for Maine Coon, Ragdoll and Sphynx cats (Figure 5), and is recommended in all breeding cats of these breeds to reduce the inheritable prevalence of HCM. It is advised that individuals homozygous for the mutation are not bred, while heterozygotes may be bred with individuals negative for the mutation 14. It is however important that breeders are aware that cats without the known genetic mutations may still develop HCM.

Figure 5. Clinicians in first-opinion practice should be alert for signs of HCM in their patients, and all feline examinations should involve careful cardiac auscultation for the presence of murmurs, gallop sounds and arrhythmias, any of which warrant further investigation. This is especially the case in breeds that are prone to cardiomyopathies, and tests are now available to detect the genetic mutation that can be responsible for HCM in the Sphynx cat.
Credit: Shutterstock
Staging of cats with HCM can help standardize treatment. No treatment is indicated for stage A and stage B1 (no/minimal left atrial dilation) cats, except in cases of severe LVOTO, in which beta-blockers may be considered (see below). Stage B2 cats are at risk of TE, and clopidogrel as a preventative therapy is advised.
As in human HCM, insulin, insulin-like growth factor-1 and inflammation have been shown to likely be implicated in the pathophysiology of feline HCM. Diet alterations targeting these factors may therefore have beneficial effects; one recent study showed that cats with pre-clinical HCM fed a diet restricted in starch and supplemented with omega-3 fatty acids had reduced LV remodeling. The advent of a commercially available feline cardiac diet now offers the veterinarian the option to choose this as a therapeutic intervention in stage B cats 23.
In people with HCM and severe LVOTO, exercise intolerance and angina are commonly reported; with improvement of clinical signs following beta blocker therapy. Their use in pre-clinical cats with evidence of LVOTO remains debatable, and the authors advise that cases are referred to a cardiologist for this decision to be made. Theoretically, beta blockers would appear favorable in cases of marked LVOTO; the negative inotropic and chronotropic effects may reduce the severity of obstruction, while also improving myocardial oxygen supply, reducing risk of arrhythmias and ischemia. However, no benefit to long-term survival nor to quality of life has been proven 24,25. Furthermore, beta blockers are contraindicated in cases of CHF and would likely be detrimental to cats close to decompensation.
Joanna Dukes-McEwan
Given that HCM has high prevalence in cats, with a tendency for a long pre-clinical phase and risk of serious clinical signs, the general practitioner should be alert for signs of stage B disease in their feline patients. All examinations should include careful auscultation for the presence of murmurs, gallop sounds and arrhythmias, any of which would warrant further investigation. Detection of stage B cats allows initiation of preventive therapy where applicable, as well as risk management prior to interventions or treatments which could precipitate decompensation. Improved owner education and vigilance may also facilitate detection of congestive heart failure prior to the development of severe respiratory compromise.
Payne JR, Brodbelt DC, Luis Fuentes V. Cardiomyopathy prevalence in 780 apparently healthy cats in rehoming centres (the CatScan study). J. Vet. Cardiol. 2015;17 Suppl 1:S244-S257.
Fox PR, Keene BW, Lamb K, et al. International collaborative study to assess cardiovascular risk and evaluate long-term health in cats with preclinical hypertrophic cardiomyopathy and apparently healthy cats: the REVEAL study. J. Vet. Intern. Med. 2018;32:930-943.
Kittleson MD, Cote E. The feline cardiomyopathies: 2. Hypertrophic Cardiomyopathy. J. Feline Med. Surg. 2021;23:1028-1051.
Cote E, MacDonald KA, Meurs KM, et al. Hypertrophic Cardiomyopathy. In: Feline Cardiology. 1st ed. John Wiley & Sons, Inc. 2011 Chapter 11;101-175.
Meurs KM, Sanchez X, David RM, et al. A cardiac myosin binding protein C mutation in the Maine Coon cat with familial hypertrophic cardiomyopathy. Hum. Mol. Genet. 2005;14:3587-3593.
Meurs KM, Norgard MM, Ederer MM, et al. A substitution mutation in the myosin binding protein C gene in Ragdoll hypertrophic cardiomyopathy. Genomics 2007;90:261-264.
Meurs KM, Williams BG, de Prospero D, et al. A deleterious mutation in the ALMS1 gene in a naturally occurring model of hypertrophic cardiomyopathy in the Sphynx cat. Orphanet J. Rare Dis. 2021;16:108.
Kittleson MD, Meurs KM, Harris SP. The genetic basis of hypertrophic cardiomyopathy in cats and humans. J. Vet. Cardiol. 2015;17 Suppl 1:S53-S73.
Schober K, Todd A. Echocardiographic assessment of left ventricular geometry and the mitral valve apparatus in cats with hypertrophic cardiomyopathy. J. Vet. Cardiol. 2010;12:1e16.
Seo J, Novo Matos J, Payne JR, et al. Anterior mitral valve leaflet length in cats with hypertrophic cardiomyopathy. J. Vet. Cardiol. 2021;37:62-70.
Maron BJ, Maron MS. A discussion of contemporary nomenclature, diagnosis, imaging, and management of patients with hypertrophic cardiomyopathy. Am. J. Cardiol. 2016;118:1897-1907.
MacLea HB, Boon JA, Bright JM. Doppler echocardiographic evaluation of mid ventricular obstruction in cats with hypertrophic cardiomyopathy. J. Vet. Intern. Med. 2013;27:1416-1420.
Novo Matos J, Pereira N, Glaus T, et al. Transient myocardial thickening in cats associated with heart failure. J. Vet. Intern. Med. 2018;32(1):48-56.
Luis Fuentes V, Abbott J, Chetboul V, et al. ACVIM consensus statement guidelines for the classification, diagnosis, and management of cardiomyopathies in cats. J. Vet. Intern. Med. 2020;34:1062-1077.
Payne JR, Borgeat K, Connolly DJ, et al. Prognostic indicators in cats with hypertrophic cardiomyopathy. J. Vet. Intern. Med. 2013;27:1427-1436.
Haggstrom J, Andersson AO, Falk T, et al. Effect of body weight on echocardiographic measurements in 19,866 pure-bred cats with or without heart disease. J. Vet. Intern. Med. 2016;30:1601-1611.
Hansson K, Haggstrom J, Kvart C, et al. Left atrial to aortic root indices using two-dimensional and M-mode echocardiography in Cavalier King Charles Spaniels with and without left atrial enlargement. Vet. Radiol. Ultrasound 2002;43(6):569-575.
Linney CJ, Dukes-McEwan J, Stephenson HM, et al. Left atrial size, atrial function and left ventricular diastolic function in cats with hypertrophic cardiomyopathy. J. Small. Anim. Pract. 2014;55(4):198-206.
Fox PR, Rush JE, Reynolds CA, et al. Multicenter evaluation of plasma N-terminal probrain natriuretic peptide (NT-pro BNP) as a biochemical screening test for asymptomatic (occult) cardiomyopathy in cats. J. Vet. Intern. Med. 2011;25:1010-1016.
Ward JL, Lisciandro GR, Ware WA, et al. Evaluation of point-of-care thoracic ultrasound and NT-proBNP for the diagnosis of congestive heart failure in cats with respiratory distress. J. Vet. Intern. Med. 2018;32:1530-1540.
Borgeat K, Sherwood K, Payne J, et al. Plasma cardiac troponin I concentration and cardiac death in cats with hypertrophic cardiomyopathy. J. Vet. Intern. Med. 2014;28:1731-1737.
Seo J, Payne JR, Novo Matos J, et al. Biomarker changes with systolic anterior motion of the mitral valve in cats with hypertrophic cardiomyopathy. J. Vet. Intern. Med. 2020;34(5):1718-1727.
van Hoek I, Hodgkiss-Geere H, Bode EF, et al. Association of diet with left ventricular wall thickness, troponin I and IGF-1 in cats with subclinical hypertrophic cardiomyopathy. J. Vet. Intern. Med. 2020;34(6):2197-2210.
Schober KE, Zientek J, Li X, et al. Effect of treatment with atenolol on 5-year survival in cats with preclinical (asymptomatic) hypertrophic cardiomyopathy. J. Vet. Cardiol. 2013;15:93-104.
Coleman AE, DeFrancesco TC, Griffiths EH, et al. Atenolol in cats with subclinical hypertrophic cardiomyopathy: a double-blind, placebo-controlled, randomized clinical trial of effect on quality of life, activity, and cardiac biomarkers. J. Vet. Cardiol. 2020;30:77-91.
Catheryn Partington
Dr. Partington graduated from the University of Liverpool in 2014, having also attained a Masters in Veterinary Science, and returned to the University for both her rotating internship and cardiology residency, completing the latter in 2021 Read more
Joanna Dukes-McEwan
Professor Dukes-McEwan graduated in 1986 from the University of Glasgow and remained there to do an internship and residency training Read more
Lungworm and heartworm are an underestimated but potentially serious threat for many cats, as this article reveals.
Diaphragmatic hernia is a common consequence of traumatic injury in cats and may be fatal if not promptly diagnosed and treated; this article reviews the pathophysiology and treatment of the condition.
Chylothorax is a differential for any cat with pleural effusion; here Elizabeth Rozanski describes her preferred approach to such cases.
Asthma is a common disease in cats, but it can mimic many other pathologies, and the diagnosis and treatment of the condition can be challenging, as this paper explains.
